Delve into the complexities of medical insurance revenue cycle management with our comprehensive guide, “medical insurance: a revenue cycle process approach epub.” This in-depth exploration provides a roadmap for optimizing your revenue cycle, maximizing efficiency, and ensuring financial stability.
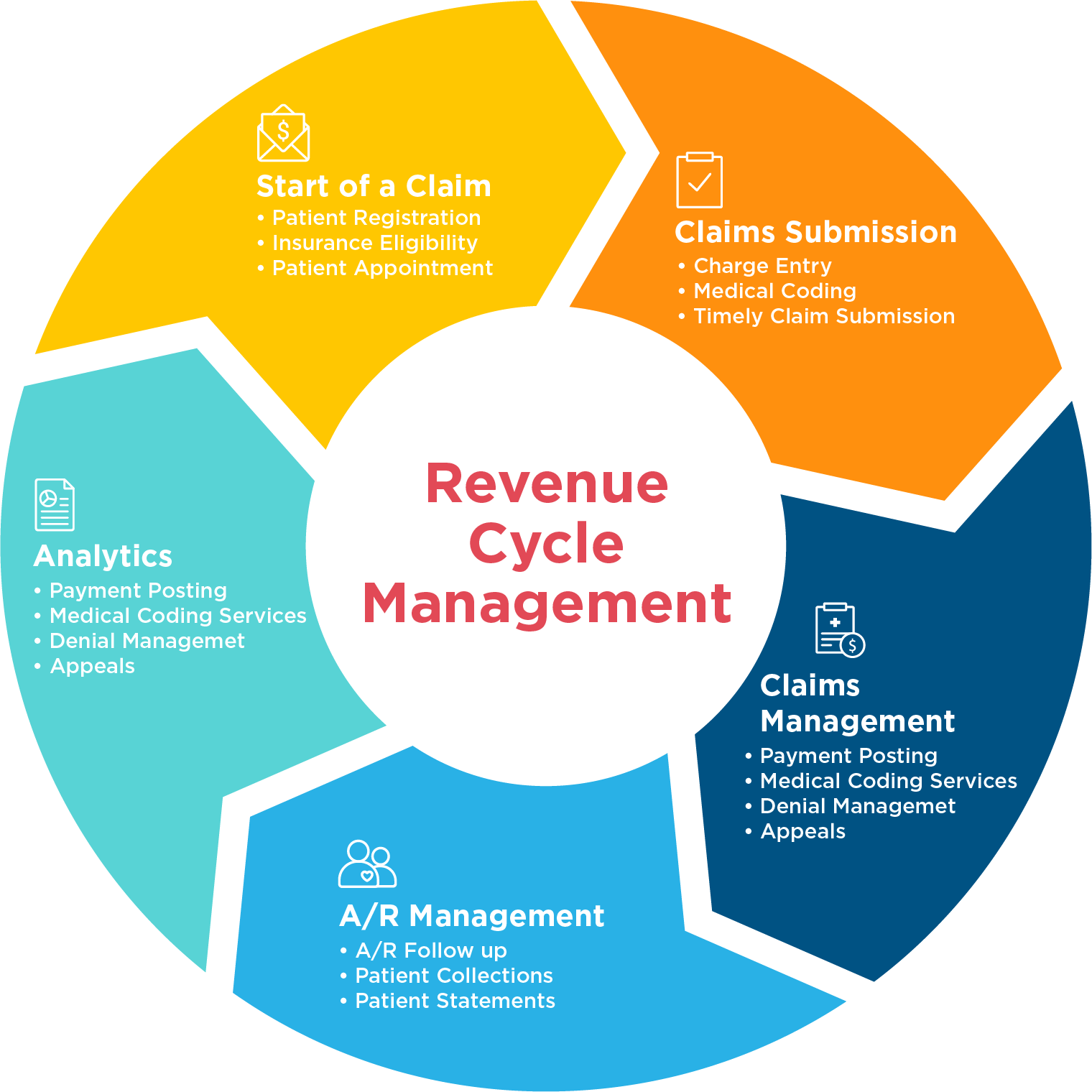
Our guide unravels the intricacies of the revenue cycle, empowering you with a thorough understanding of its key components, stakeholders, and processes. From patient registration to claim submission and denial management, we delve into each step, equipping you with the knowledge and strategies to streamline your operations.
Medical Insurance Revenue Cycle: An Overview

The medical insurance revenue cycle is the process by which healthcare providers receive payment for the services they provide to patients. The revenue cycle begins when a patient schedules an appointment and ends when the provider receives payment for the services rendered.
The revenue cycle is a complex process that involves multiple stakeholders and a variety of processes.
The key components of the medical insurance revenue cycle include:
- Patient registration
- Scheduling
- Claims processing
- Payment posting
- Collections
The different stakeholders involved in the revenue cycle include:
- Patients
- Providers
- Insurance companies
- Billing companies
- Collection agencies
The key processes involved in the revenue cycle include:
- Patient registration
- Scheduling
- Insurance verification
- Claims submission
- Payment posting
- Collections
Charge Capture and Coding
Charge capture and coding are critical steps in the medical insurance revenue cycle. Charge capture involves identifying and documenting all services provided to a patient, while coding assigns standardized codes to these services for billing purposes.
Accurate coding is essential for ensuring that the correct amount is billed to the patient and the insurance company. Incorrect coding can lead to denied claims, delayed payments, and even legal issues.
Common Coding Errors
- Using incorrect codes for the services provided
- Omitting necessary codes
- Using codes that are not specific enough
- Using codes that are not supported by the medical record
- Using codes that are not compliant with insurance regulations
Claim Submission
Claim submission is the process of submitting a request for payment to a health insurance company for covered medical services. It involves gathering and organizing patient information, medical records, and other necessary documentation to support the claim.
There are different types of claims that can be submitted, including:
- Professional claims: These claims are submitted by healthcare providers for services they have provided to patients, such as doctor visits, surgeries, and diagnostic tests.
- Institutional claims: These claims are submitted by hospitals and other healthcare facilities for services they have provided to patients, such as inpatient stays, outpatient surgeries, and emergency room visits.
- Pharmacy claims: These claims are submitted by pharmacies for prescription drugs that have been dispensed to patients.
It is important to submit claims timely and accurately to ensure that patients receive the benefits they are entitled to and that healthcare providers are reimbursed for the services they have provided. Late or inaccurate claims can result in delays in payment or even denial of claims.
Obtain a comprehensive document about the application of best gravel bikes 2023 under 1000 that is effective.
Reporting and Analytics
Reporting and analytics are crucial components of the medical insurance revenue cycle. They provide valuable insights into the performance of the revenue cycle and identify areas for improvement.
The reporting and analytics process involves collecting, analyzing, and interpreting data from various sources within the revenue cycle. This data can include information on patient demographics, claims processing, denials, and collections.
Types of Reports
Various types of reports can be generated to provide insights into the revenue cycle. Some common types of reports include:
- Financial reports:These reports provide an overview of the financial performance of the revenue cycle, including revenue, expenses, and profitability.
- Operational reports:These reports provide insights into the operational efficiency of the revenue cycle, including the time it takes to process claims and the number of denials.
- Performance reports:These reports evaluate the performance of individual staff members and teams involved in the revenue cycle.
Importance of Data
Data is essential for improving the revenue cycle. By analyzing data, healthcare providers can identify trends, patterns, and areas for improvement. This information can be used to make informed decisions about process changes, technology investments, and staff training.
For example, if a healthcare provider analyzes data and finds that a large number of claims are being denied due to coding errors, they can implement training programs to improve the accuracy of coding.
Technology and the Revenue Cycle
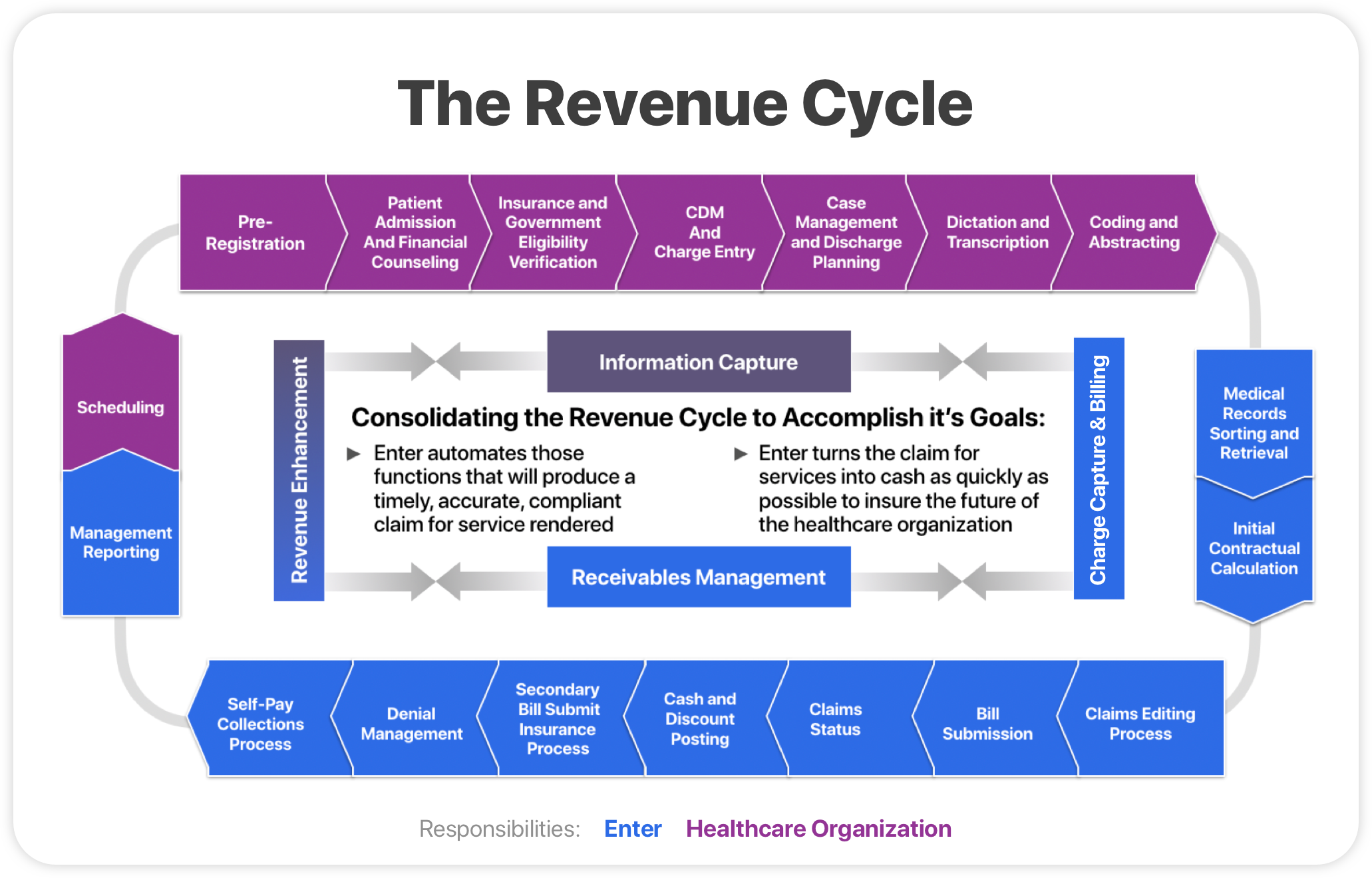
Technology plays a crucial role in enhancing the efficiency and accuracy of the revenue cycle process. By automating tasks, improving data management, and ensuring data security, technology can significantly streamline operations and reduce administrative costs.
Types of Technology Used in the Revenue Cycle
Various types of technology can be utilized to improve the revenue cycle, including:
- Electronic Health Records (EHRs):Centralize patient health information, enabling seamless data sharing and improving communication between healthcare providers.
- Practice Management Systems (PMSs):Manage patient scheduling, billing, and insurance claims, automating tasks and reducing manual errors.
- Revenue Cycle Management (RCM) Software:Automates and optimizes the entire revenue cycle process, including claims processing, payment tracking, and reporting.
- Artificial Intelligence (AI) and Machine Learning (ML):Analyze data, identify patterns, and predict outcomes, improving decision-making and automating complex tasks.
Benefits of Using Technology in the Revenue Cycle
Automating tasks using technology offers several benefits:
- Increased efficiency:Automating repetitive and time-consuming tasks frees up staff for more complex tasks, enhancing productivity.
- Improved accuracy:Automated systems reduce the risk of human error, ensuring accurate billing and claims processing.
li> Reduced costs:Automating tasks reduces labor costs and improves operational efficiency, leading to overall cost savings.
Data Security and Privacy
While technology offers numerous benefits, it is essential to prioritize data security and privacy. Healthcare organizations must implement robust security measures to protect sensitive patient information, such as:
- Encryption:Encrypting data ensures that unauthorized individuals cannot access it.
- Access controls:Limiting access to data to authorized personnel reduces the risk of data breaches.
- Regular security audits:Conducting regular security audits identifies vulnerabilities and ensures compliance with regulations.
Best Practices for Medical Insurance Revenue Cycle Management
Medical insurance revenue cycle management is a complex process that can be challenging to navigate. By following best practices, healthcare organizations can improve efficiency, profitability, and patient satisfaction.
For descriptions on additional topics like uzip electric bike rentals, please visit the available uzip electric bike rentals.
Some of the best practices for medical insurance revenue cycle management include:
- Establish clear policies and procedures.Having clear policies and procedures in place will help to ensure that all staff members are following the same processes and that there is consistency in the way that claims are processed.
- Use technology to automate tasks.There are a number of software solutions available that can help to automate tasks such as claim submission, eligibility verification, and payment posting. This can free up staff time to focus on more value-added activities.
- Outsource non-core functions.Outsourcing non-core functions such as claims processing or billing can help to reduce costs and improve efficiency.
- Monitor key performance indicators.Tracking key performance indicators such as days in accounts receivable and net collection rate can help to identify areas for improvement.
- Educate patients about their financial responsibility.Patients need to be aware of their financial responsibility for their medical care. Educating patients about their insurance coverage and payment options can help to reduce the number of unpaid claims.
By following these best practices, healthcare organizations can improve the efficiency of their revenue cycle and increase profitability.
Examples of Successful Implementation, Medical insurance: a revenue cycle process approach epub
There are a number of healthcare organizations that have successfully implemented best practices for medical insurance revenue cycle management. One example is the Cleveland Clinic. The Cleveland Clinic has implemented a number of initiatives to improve its revenue cycle, including:
- Centralizing its billing operations
- Automating claim submission and payment posting
- Outsourcing non-core functions
- Educating patients about their financial responsibility
As a result of these initiatives, the Cleveland Clinic has improved its days in accounts receivable by 10% and its net collection rate by 5%.
Closing Notes: Medical Insurance: A Revenue Cycle Process Approach Epub
In conclusion, “medical insurance: a revenue cycle process approach epub” serves as an indispensable resource for healthcare professionals seeking to enhance their revenue cycle management practices. By implementing the best practices Artikeld within, you can optimize your processes, improve profitability, and deliver exceptional patient care.
FAQ Compilation
What are the key components of the medical insurance revenue cycle?
The medical insurance revenue cycle encompasses patient registration, charge capture, coding, claim submission, payment processing, denial management, patient billing, reporting, and analytics.
How can I improve the efficiency of my revenue cycle?
Implementing technology, automating tasks, and following best practices can significantly enhance the efficiency of your revenue cycle.
What are the common errors to avoid in medical coding?
Incorrect patient information, inaccurate procedure codes, and missing modifiers are some common coding errors that can lead to claim denials.
